Failure to thrive (FTT)
Children who fail to gain weight adequately have a disorder known as failure to thrive. This needs to be differentiated from newborns who lose weight initially. In the first week of life, it is normal to lose 5-10% of the birth weight. By 2-3 weeks, most of these babies surpass their birth weights and are on their way to gain 25-35 grams of weight daily. From 4-6 months babies gain on average 10-20 grams and this number drops even further to 5-10 grams after 6 months. To diagnose FTT one of the below needs to be true:
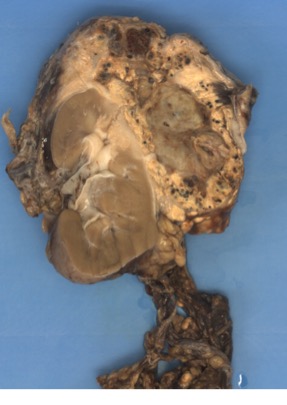
- An infant that is less than 5th percentile for weight for a given age
- An infant that is less than 5th percentile for weight in length for a given age
- An infant whose weight is between the 9th and 91st percentile, but manages to cross more than 2 major percentile lines on the standard infant growth chart as shown below
Picture 1. CDC growth chart for 36-month-old males
Causes
Causes of FTT are divided into organic and non-organic causes. Organic causes are usually those that can be reversed by treating the underlying disease (mental, or the physical issues with the child itself), while the non-organic causes are caused by the caregiver's actions and require behavioral changes to be reversed. It is estimated that organic causes make up less than 10% of FTT etiologies.
| Organic causes | Non-organic causes |
| GI system problems | Physical inability to produce breastmilk |
| Cystic fibrosis | Not feeding enough at 2-3 hour intervals |
| Metabolic disorders | Neglect |
| Liver disease | Poverty |
| Anemia | Inadequate duration of feeds (10-30 mins at a time is normal) |
| Iron deficiency | |
| Inflammatory bowel disease |
Sometimes failure to thrive is a mix of these 2 causes and is known as a mixed type of failure to thrive. In many cases of FTT no specific cause is found.
Finding the cause
In babies suspected to have a non-organic FTT disorder, it is important to have a detailed history from the caregiver. These include the baby's birth weight, source of food (breast milk vs formula), frequency and duration of the feeding, problems latching on, difficulty producing milk, mental issues and stress (postpartum depression) experienced by the caregiver, number of other children, support network of the caregiver and many others.
Organic causes manifest within the baby and can show rather obvious signs on history and physical exam.
- History signs
- Birth weight
- Weight gain or loss since birth
- Signs of respiratory illnesses
- Other siblings with FTT
- Family history of FTT
- Lethargy during feeds
- Physical exam signs
- Vital signs - check for sepsis
- High respiratory rate (normal is between 40 and 60 per minute)
- Tachycardia
- Hypotension
- Fever
- Cardiac exam
- Murmurs - present in up to 50% of newborns, mostly benign and disappear within hours to weeks
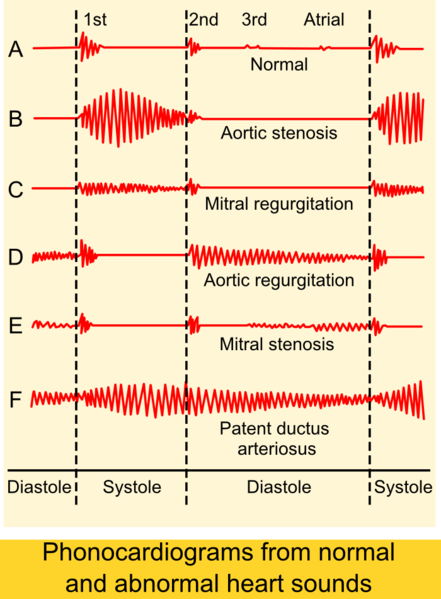
- Diastolic murmurs are always pathological (caused by mitral/tricuspid stenosis, aortic/pulmonary regurgitation)
- Grades 4-6 murmurs are likely to be pathologic and require a cardiologist assessment
- Patent ductus arteriosus (PDA)
- Marked by a continuous murmur
- Important questions to ask about murmurs - if the answer to all of this is 'no', the murmur is considered benign.
- Is the child well?
- Is the murmur diastolic?
- How is precordial activity?
- Is the grade of murmur 2 or less?
- Is oxygen saturation normal? Is the baby acyanotic?
- Is the second heart sound split normally?
- Pulses
- Differences between arms, or arms and lower limbs can signify aortic coarctation
- Congestive heart failure and a murmur in an infant can be caused by
- VSD
- Severe aortic stenosis
- Coarctation of the aorta
- PDA
- Murmurs - present in up to 50% of newborns, mostly benign and disappear within hours to weeks
- Abdominal exam
- Organomegaly
- Hepatomegaly (normal should be palpated 1cm below the right costal margin in young infants)
- Sign of congestive heart failure in children
- Caused by decreased renal blood flow>Renin angiotensin system activation>fluid retention and systemic venous congestion
- Differential diagnosis
- Congestive heart failure
- Dyspnea with feeding
- Diaphoresis
- FTT
- Active precordium
- Hepatomegaly
- Hepatitis
- Congenital infections
- Inborn metabolic errors
- Anemias
- Tumours
- Congestive heart failure
- Hepatomegaly (normal should be palpated 1cm below the right costal margin in young infants)
- Masses
- Nephroblastoma - known as Wilms tumour
- Neuroblastoma - within the adrenal glands
- Nephroblastoma - known as Wilms tumour
- Organomegaly
- Vital signs - check for sepsis
Treatment
If underlying conditions in either the parent or the infant are diagnosed, treating them is a good place to start. However, sometimes problems can persist despite having managed the primary underlying condition. Referral to a psychologist is recommended when behavioral issues are affecting the child's nutrition status. In severe cases of FTT, special care must be taken to avoid refeeding syndrome, which is caused by a shift of fluid and electrolytes in a severely malnourished person that can potentially be fatal.
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.